Health Byte 002: How Startups are Moving the Needle on America's Obesity Epidemic
Startups are embracing integrated approaches to provide patient-centered solutions for obesity.
Background
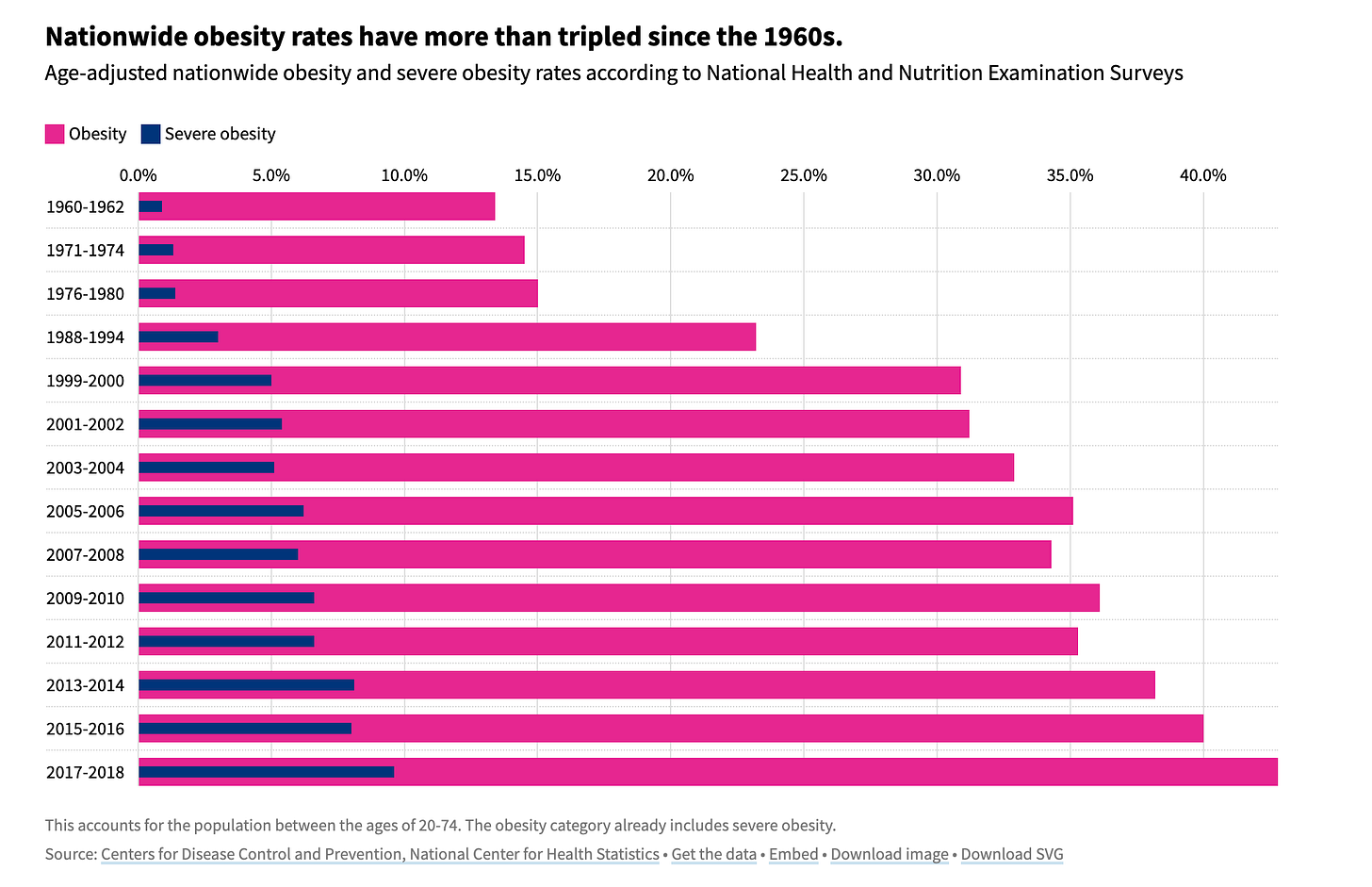
🇺🇸 America has a problem — and I’m not just referencing 👑 Queen Bey’s stellar song from the Reinassance album. I’m talking about the sobering statistics about this country’s dangerously expanding obesity crisis. This public health issue isn’t fading gently into the background either as the trends grow increasingly grim.
Source: CDC-NCHS and USA Facts
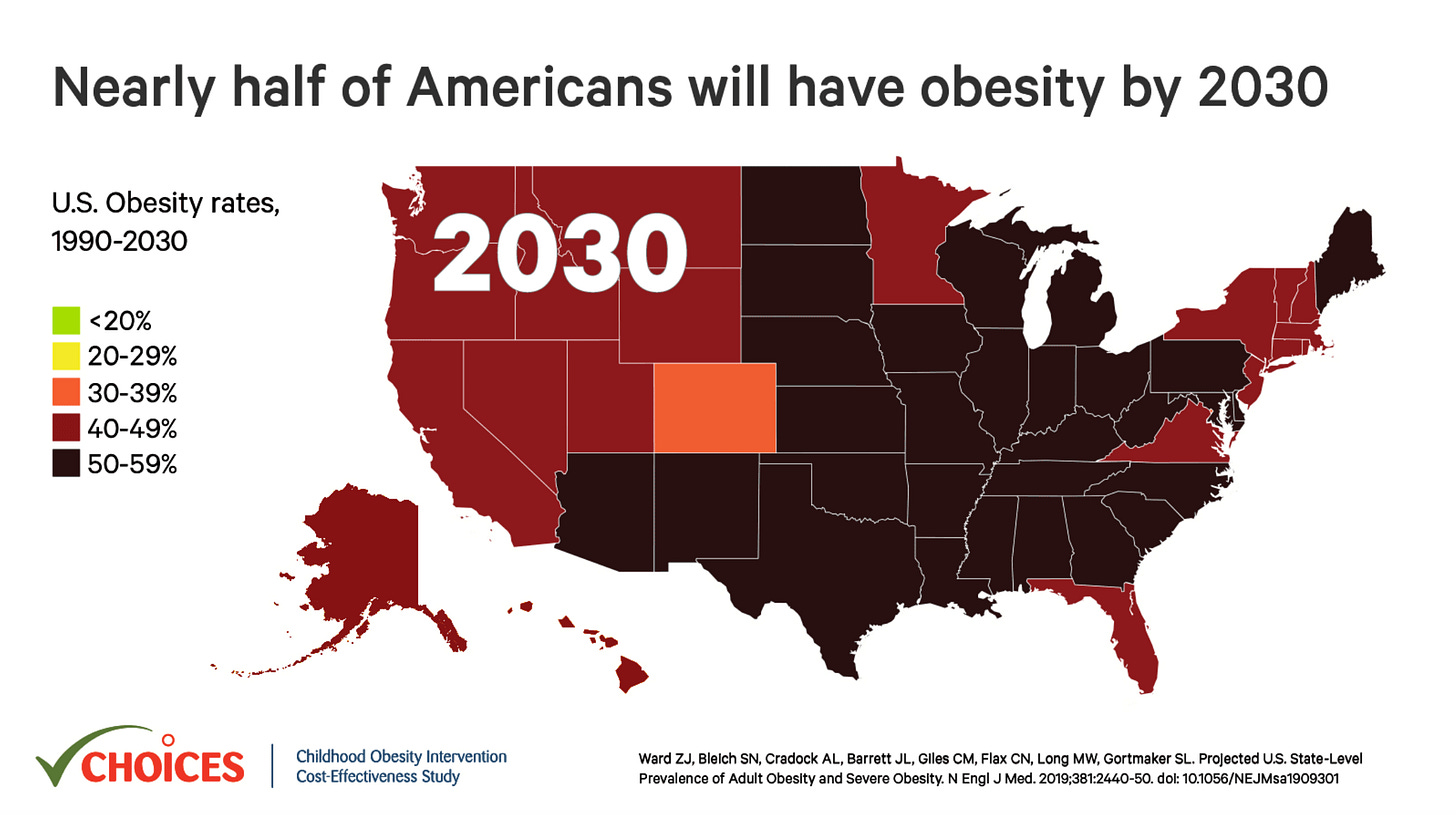
Currently, slightly over 40% of adults in the United States meet the criteria for clinical obesity; however, if current trends continue, projections estimate approximately 50% of American adults—close to half the population—will be obese by the year 2030.
Source: The Choices Project
Certain demographic segments bear a disproportionate burden. Research studies indicate that Black and Latino adults experience particularly high obesity rates, reaching approximately 50% and 46%, respectively. Geographic disparities exist too, with individuals living in rural areas facing heightened levels of obesity compared to those in urban and suburban settings. These jarring health inequities demonstrate how obesity cannot be boiled down to just bad individual lifestyle decisions. Rather, one's risk relates deeply to the social determinants of health – the environmental and social conditions that people are born into and navigate daily.
Source: Global Health News Wire
From accessibility of affordable nutritious foods, proximity to safe exercise venues, targeted marketing of unhealthy products, workplace wellness cultures, and healthcare system barriers, the environments individuals inhabit either empower healthy choices or stack the deck against them. This explains why marginalized racial, ethnic, and rural groups face considerably heightened obesity risks – their living contexts too often systematically deny health-promoting options that others take for granted. The stakes feel immense at both individual and societal levels. And costs will only snowball if current trends continue – the CDC pins obesity-related healthcare expenditures at a whopping $147 billion annually as rates of associated chronic illnesses like diabetes and heart disease show no signs of plateau. With complexity piled upon complexity fueling the obesity crisis, can innovative solutions shift trajectories to promote health equity?
Key Drivers
▶️ Failure of America’s Food System
Inequities in access to healthy, affordable food options help drive high obesity rates in the United States. Low-income areas often lack grocery stores selling fresh produce or other healthier items instead relying on convenience and fast food outlets. Government subsidies disproportionately support the production of unhealthy processed foods and animal products over fruits, vegetables, and whole grains. These systemic inequities make consuming a nutritious diet challenging, especially for many lower-income communities of color, as they are constantly bombarded with ads for ultra-processed food and beverages high in sugar, unhealthy fats, and sodium. With diet closely tied to risks for obesity and related diseases, transforming food systems to promote equity must be part of efforts to combat the obesity epidemic, including looking at advertising regulations. Achieving a meaningful shift requires addressing pervasive junk food marketing and making healthy, affordable options more available in all communities.
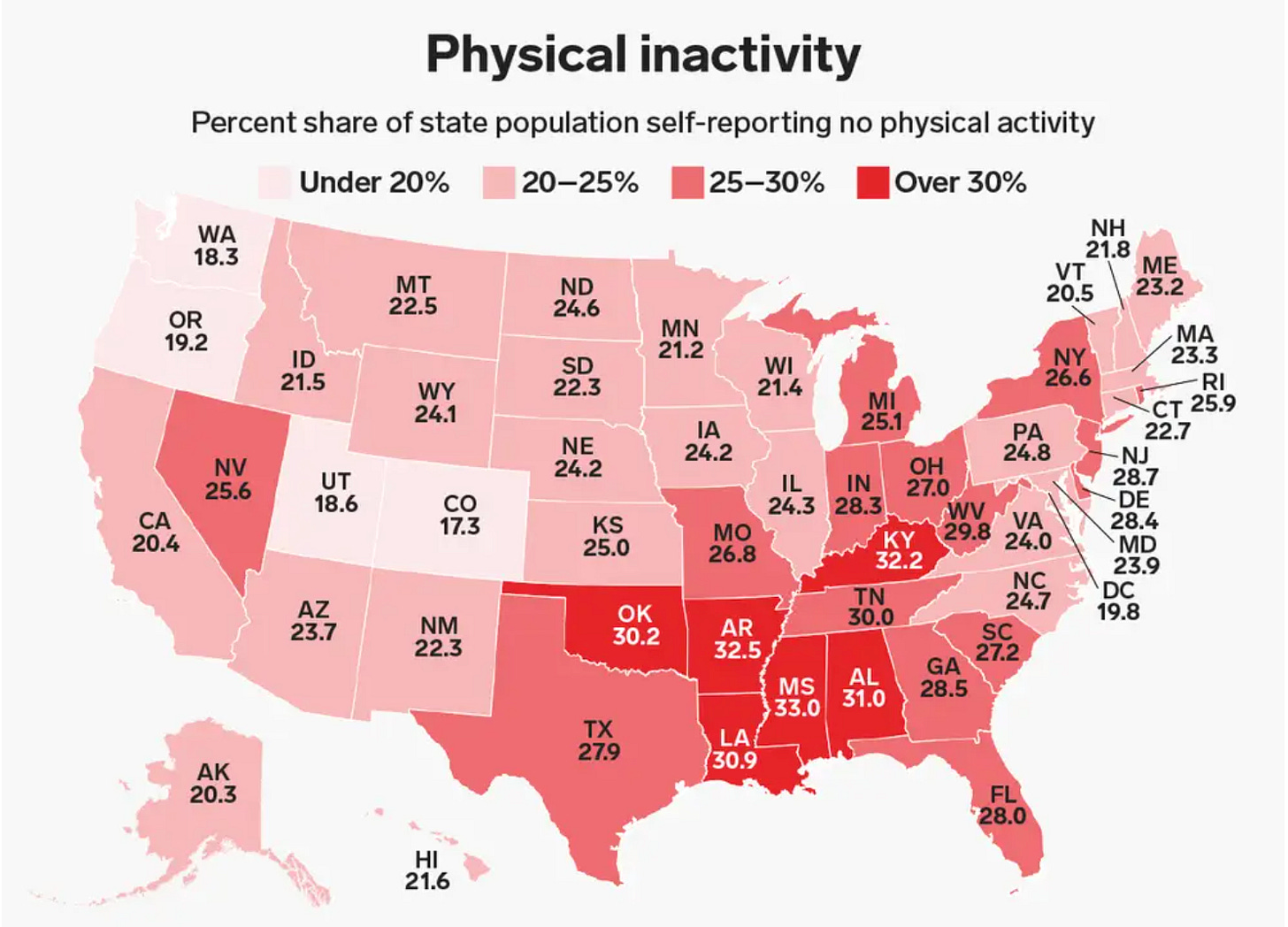
▶️ Lack of Physical Activity
Source: Business Insider and Center for Disease Control and Prevention
Sedentary lifestyles have become more prevalent across the United States, with recent statistics revealing troubling rates of physical inactivity. A nationwide study in 2020 found that every state had at least 15% of US adults reporting being physically inactive. Additionally, southern states like Oklahoma, Tennessee, Arkansas, Mississippi, Louisiana, Alabama, and Kentucky exceeded 30% adult inactivity rates. This growing physical inactivity is likely fueled by several modern societal factors. Increased daily screen time from TV, smartphones, video games, and computers fosters sedentary habits that begin in childhood, as evidenced by the average of 10.5 hours per day that U.S. adults spend connected to media devices. Excessive sitting and lack of movement are also associated with disrupted sleep patterns and shorter sleep duration, compounding health risks. Additionally, the shift toward automobile-centric infrastructure and stationary desk jobs has reduced physical activity levels by discouraging other forms of transportation like biking and replacing labor-intensive work with prolonged sitting, contributing to weight gain over time.
▶️ Genes matter, but behavior and nutrition matter more
Source: Bart - stock.adobe.com
Because genetic shifts in human populations typically happen over longer periods, they do not explain the fast upsurge in obesity prevalence seen in just the past few decades. So while genetics are not the root cause of the obesity epidemic, they do still play a contributing role. Research shows that people vary substantially in how their weight, appetites, and metabolisms respond to the same diets and lifestyles. Some of this variation can be attributed to genetic differences. For instance, certain gene variants make some individuals more prone to overeating, craving high-calorie foods, and storing excess calories as fat. However, for most people, weight management remains possible through diet and lifestyle changes. The sheer speed of growth in obesity rates indicates that behavioral and environmental shifts like increased access to processed foods and sedentary lifestyles are likely the predominant drivers of this crisis. Still, understanding genetic influences can help medical providers better support those who are biologically more susceptible to obesity with targeted solutions. Appreciating all influencing factors - including but not limited to genetics - will be important for overcoming this public health challenge.
Market Potential and Growth
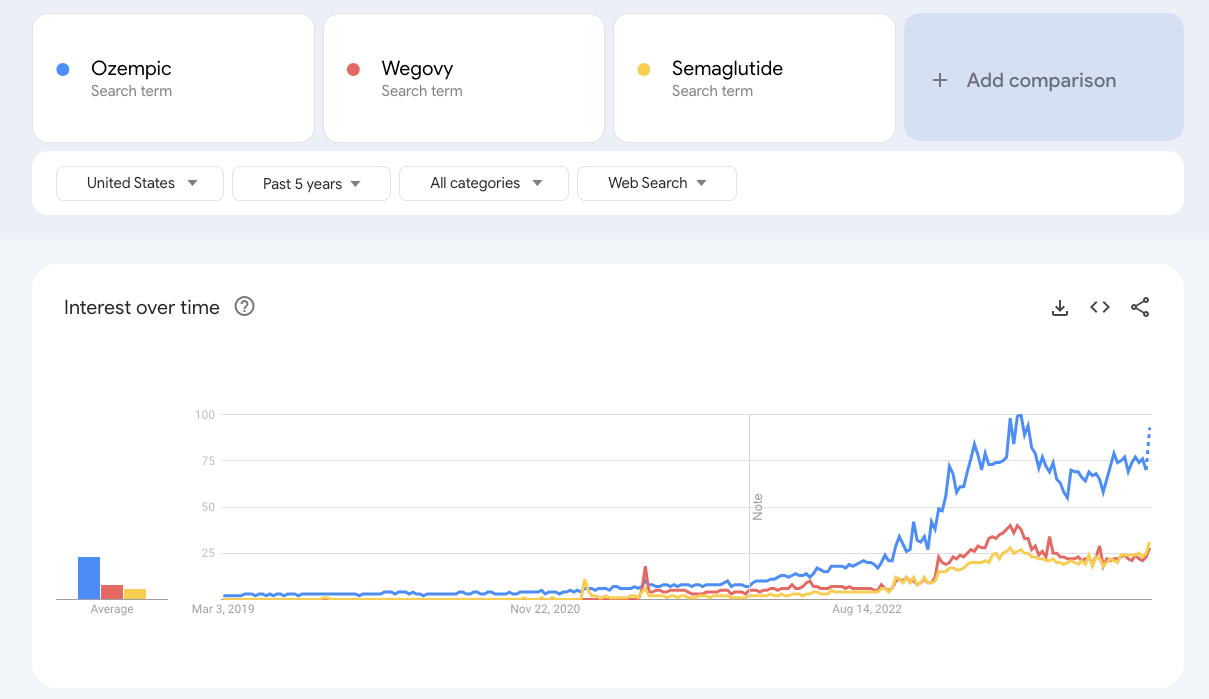
Drug treatments for obesity are not a new idea. One type that has recently gained immense popularity is called GLP-1s (Glucagon-like peptide-1). To put it simply for non-scientists, GLP-1 is a hormone that helps regulate appetite and food intake. GLP-1 medicines like semaglutide (sold under brand names like Ozempic and Wegovy) work by mimicking this hormone’s effects. Though GLP-1 drugs have been studied since the 1980s, they only truly took off in recent years after semaglutide won FDA approval for treating both type-2 diabetes and obesity. While Wegovy is FDA-approved for weight loss in patients with obesity, Ozempic is approved to treat type 2 diabetes. However, some healthcare providers have increasingly prescribed Ozempic off-label to aid weight loss as well.
Source: Google Trends
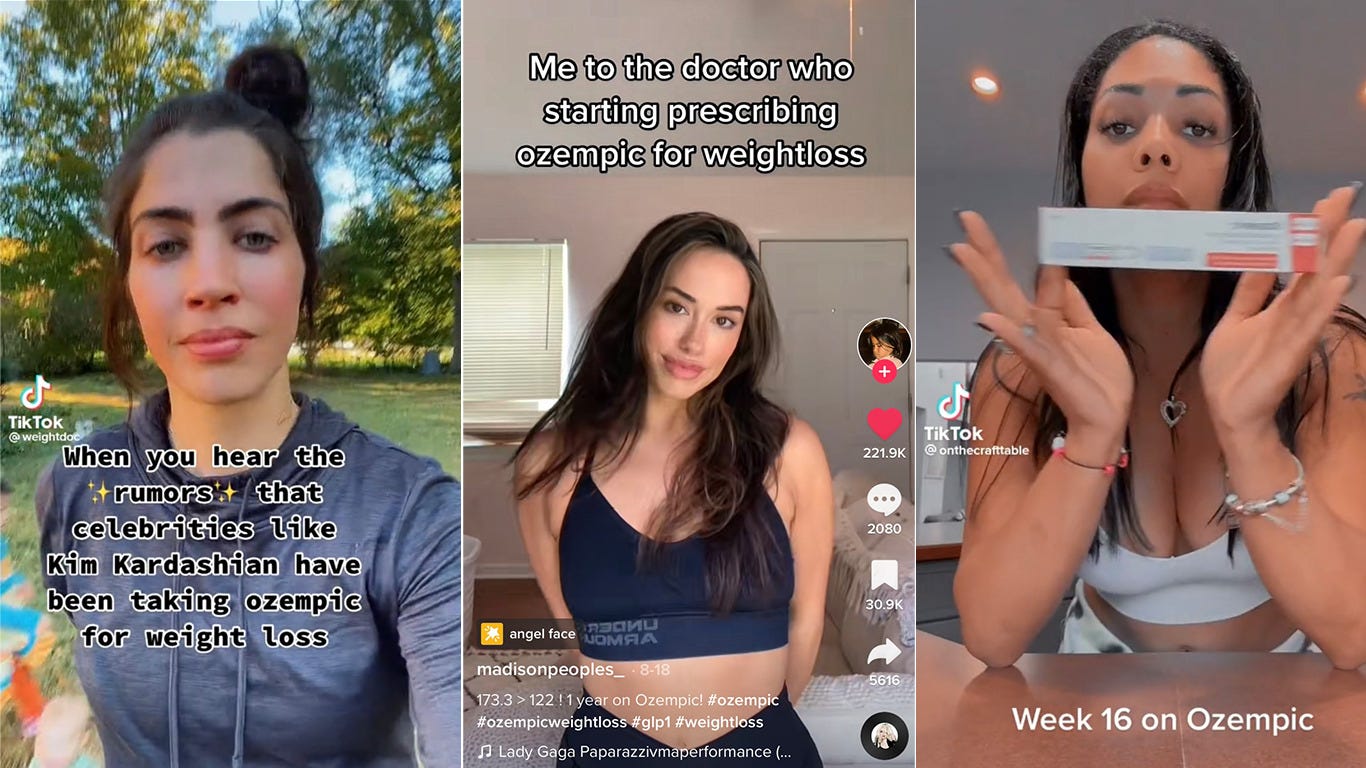
The impact has been enormous - these injections are reaching a far wider population than their original creators envisioned. Platforms like TikTok are filled with people documenting their personal weight loss journeys using Ozempic, providing influential before-and-after transformations and weight fluctuations for all to see. The hashtag #ozempic has received nearly 300 million views alone on TikTok. This level of accessible, personable connection and endorsement from real users has driven exceptional awareness and interest in trying the drug among the wider public. Through sharing their first-hand experiences, social media users have accelerated semaglutide's expansion as a weight management phenomenon beyond clinics and directly into the consumer consciousness.
Source: The Jut
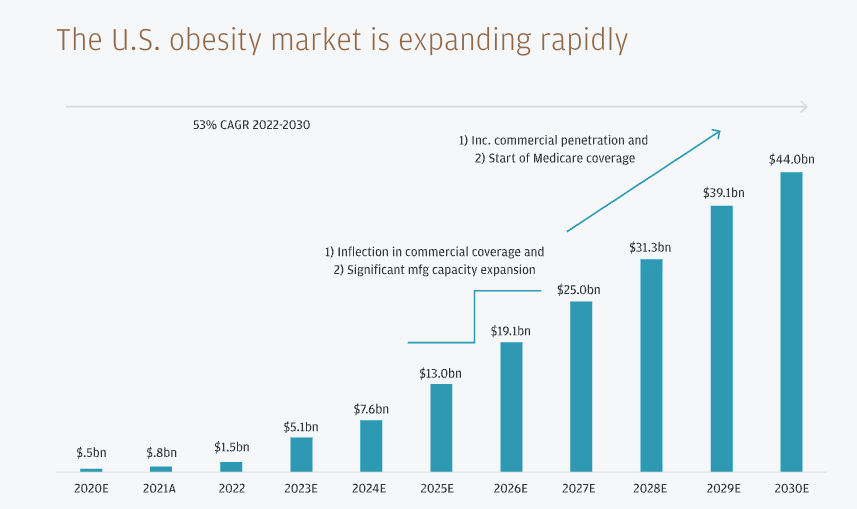
Sensing massive opportunities, weight management startups have rushed to incorporate GLP-1s into treatment offerings. With obesity rates showing no signs of slowing, the market growth possibilities for semaglutide and molecules like it appear tremendous moving forward: J.P. Morgan Research has forecasted these drugs could reach over $100 billion in global sales by 2030. They predict this growth to be powered in near equal measure by demand from diabetes and obesity treatment. In the United States specifically, they estimate the number of patients using GLP-1 drugs could swell to 30 million by 2030.
Source: JP Morgan Research
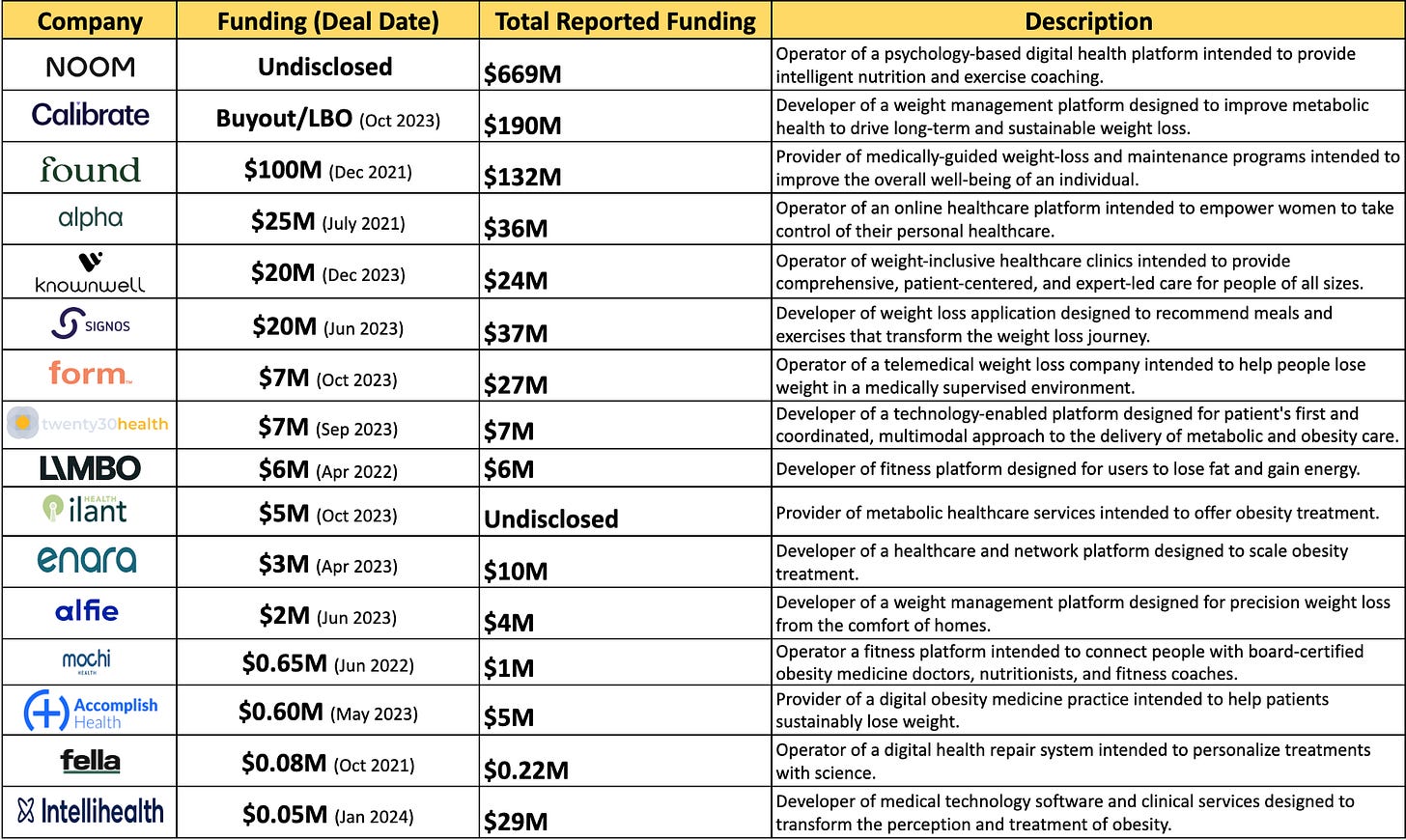
While extremely effective, GLP-1 medications alone are not a one-stop solution for resolving obesity. Weight management is complicated and multi-faceted — requiring behavior change, improved nutrition, exercise, emotional support, and more alongside pharmaceutical therapies. Recognizing this complexity, venture-backed startups are increasingly entering the weight management space to provide comprehensive solutions. At the same time, traditional players like Weight Watchers, who previously focused heavily on diet and fitness, are having to reimagine their offerings as well. The most promising weight management companies will realize pharmaceuticals alone cannot tackle obesity. Sustainable approaches will integrate lifestyle modification tools like coaching and peer support with medications like GLP-1s. Leading digital health startups in this space are already bringing more holistic chronic disease viewpoints into comprehensive offerings that address root drivers of behavior and nutrition. These multidimensional solutions signify the new standard needed for obesity improvement.
Startups to Watch
*While highlighting key players, the preceding chart does not encompass the complete landscape of weight management startups.
Source: Pitchbook
Some weight management startups are taking a value-based care approach, which aligns incentives around improving patient outcomes relative to healthcare costs. Founders like Elina Onitskansky of Ilant Health and Rajesh Aggarwal MD, PhD of twenty30 Health are turning to value-based care models. This approach helps with differentiation in a fragmented market, allowing quality-focused care rather than competition on cost or fad diets. Though value-based care companies take on some outcome risks, they also stand to benefit from higher reimbursements if they succeed at improving obesity rates - making it a potentially sustainable model. Given the immense economic and social costs of conditions like obesity, these founders recognize rethinking traditional healthcare can provide holistic solutions while benefiting their business.
With childhood obesity reaching epidemic proportions in the US - impacting a staggering 1 in 5 youth - other weight management companies have scaled out their offerings for younger demographics in need. Founders like Brooke Boyarsky Pratt of knownwell have expanded services to target adolescents living with obesity. However, legacy players like Weight Watchers faced major backlash and legal complaints after controversially acquiring children's weight loss app Kurbo in 2019. Critics condemned the promotion of dieting mentalities to impressionable youth on the Kurbo app. Additionally, post-acquisition lawsuits alleged Weight Watchers had illegally collected personal information from minors without parental consent. With an ethical and inclusive approach reflecting Pratt’s firsthand perspective, knownwell stands better positioned to address childhood obesity compared to past players who ultimately sparked criticism and litigation after failing to put kids' wellbeing first.
Several later-stage digital health companies are making moves into the weight management industry. Everly Health recently expanded its virtual care offerings to include a new weight loss program featuring GLP-1 medications for eligible patients along with testing, treatment, and ongoing support. WeightWatchers also entered the prescription weight loss space through its acquisition of Weekend Health, aiming to incorporate GLP-1 medications into its offerings. Additionally, Ro launched the Ro Body Program with access to GLP-1 drugs, while Hims & Hers rolled out a supplemental weight loss program intending to provide GLP-1 medications down the line.
Risk Factors to Consider
💸💸 Despite strong evidence of their effectiveness, some major employers and insurers like Ascension, the University of Texas System, and the North Carolina State Health Plan have begun outright excluding these prescriptions from coverage. Others like the Mayo Clinic are establishing strict prior authorization policies on who they will cover them for. While demand for GLP-1 medications has grown substantially, increasingly selective insurance coverage threatens to limit access mainly to those who can afford high out-of-pocket costs. This presents a challenge for many patients who could benefit from these medications but face financial barriers to access.
🔍 🩺 Health professionals have criticized the lack of medical oversight and misleading advertising by weight loss companies like NextMed and WeightWatchers: By using influencers and actors who have never actually taken the weight loss drugs to promote them, these companies erode consumer trust and prioritize profits over appropriate patient care. Other digital health startups should be wary of replicating these questionable advertising and prescribing practices if they want to build consumer trust and demonstrate responsible oversight of prescription medications.
🤢😔 GLP-1 drugs come with side effects like nausea and gastrointestinal distress. They also often lead to weight regain when patients stop taking them if lifestyle habits remain unchanged. Long-term diet and activity modifications are key to maintaining weight loss over time. The most responsible and sustainable business models among weight management startups will be those that provide holistic solutions beyond just prescribing drugs. Companies narrowly focused on aggressively selling GLP-1s risk backlash for failing to set realistic patient expectations and the importance of lifestyle changes for keeping weight off. The obesity epidemic demands more thoughtful and multifaceted approaches than pharmaceutical quick fixes alone.
Key Takeaway
Obesity is a complex health issue, but weight management startups are pioneering new approaches including GLP-1 medications. While these drugs show promise, the most sustainable business models will take an integrated approach beyond just prescribing. Startups focused on overall patient health will combine lifestyle coaching on diet and physical activity with medications as needed. They'll also set realistic expectations on efficacy and side effects instead of overpromising a pharmaceutical quick fix. The obesity epidemic has no one-size-fits-all solution - it demands patient-centered, holistic care anchored around evidence-based interventions for lasting outcomes.
What I'm Reading, Watching, and Listening To…
🤓 Article - Information is a determinant of health
📖 Book Recommendation - Unmasking AI: My Mission to Protect What Is Human in a World of Machines by Joy Buolamwini
📺 TV - Avatar: The Last Airbender
🎙Podcast - How Getting Active Can Make You Happier (The Happiness Lab with Dr. Laurie Santos)
🎶 Music - Texas Hold’Em by Beyoncé